Cervical cancer
Key facts
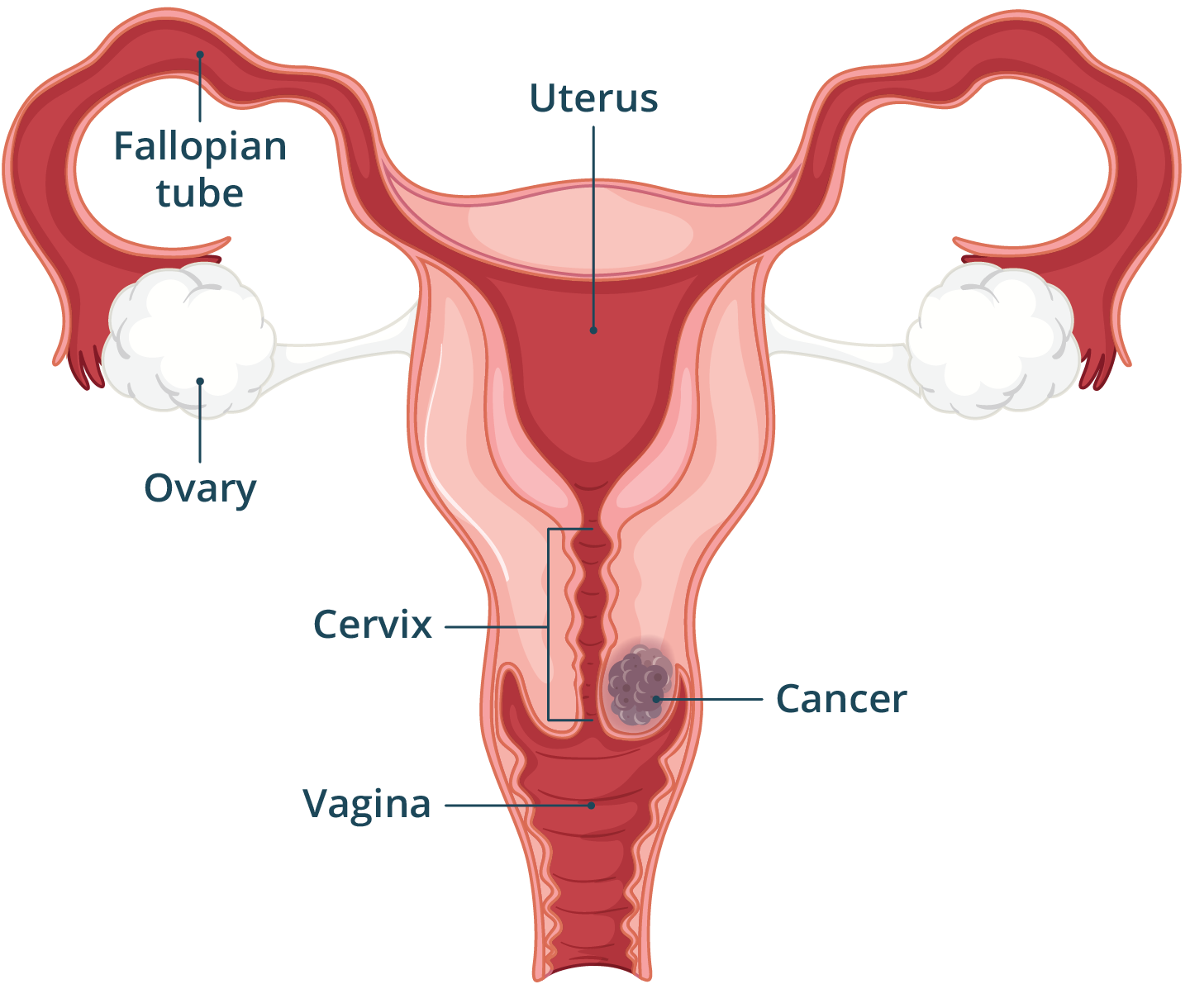
- Cervical cancer affects the cervix, which is the entrance to the uterus from the vagina.
- It is usually caused by certain types of human papilloma virus (HPV) that can lead to cancer over time.
- Most high-risk types of HPV can be prevented by the HPV vaccine.
- Regular cervical screening tests can find early changes that could lead to cancer.
- Early detection of cervical cancer can lead to a good prognosis.
What is cervical cancer?
Cervical cancer is cancer that begins growing in or on the cervix, the neck of the uterus (womb). Cancer happens when cells grow and spread in an uncontrolled way.
There are two main types of cervical cancer, depending on which cells are affected:
- Cervical squamous cell carcinoma is cancer of the flat cells on the surface of the cervix. It makes up about two thirds of all cervical cancer cases.
- Cervical adenocarcinoma affects the cells that produce mucus in the cervix. It makes up about one third of cases.
What are the symptoms of cervical cancer?
In its early stages, cervical cancer may cause very few symptoms or none at all.
Common early symptoms of cervical cancer include:
- unexpected vaginal bleeding, such as between periods, after menopause or after sex
- heavier or longer periods than usual
- unusual vaginal discharge
- pain in the lower belly (pelvis)
- pain during sex
Symptoms of more advanced cancer, which are less common, include:
CHECK YOUR SYMPTOMS — Use the Symptom Checker and find out if you need to seek medical help.
What causes cervical cancer?
Cervical cancer happens when something causes the cells in the cervix to change and grow uncontrollably. The most common cause is infection with a virus called human papillomavirus (HPV).
HPV infection
Most cervical cancers happen after an infection with certain types of HPV. About 4 in 5 people will be infected with at least one type in their lives. HPV is usually passed on during sexual contact with someone who has the virus.
Most people who get HPV will have no symptoms and the virus will be destroyed by their immune system. In some people, the virus stays in the body and can cause changes in the cervix. These changes happen slowly — usually over years — and can lead to cancer.
Other risk factors
While HPV is the main cause of cervical cancer, other factors can also increase your risk, such as:
- smoking or being around smokers
- long-term use of the oral contraceptive pill
- a weakened immune system
- exposure to a chemical called DES (a medicine used in the 1950s to prevent miscarriage)
- a family history of cervical cancer
- age over 35 years
When should I see my doctor?
You should see your doctor if you have unexpected vaginal bleeding, a change in your vaginal discharge or pelvic pain.
These symptoms can also be caused by conditions other than cancer. If you’re worried, your doctor can give you advice or refer you for tests.
FIND A HEALTH SERVICE — The Service Finder can help you find doctors, pharmacies, hospitals and other health services.
How is cervical cancer diagnosed?
Cervical cancer can be diagnosed after a positive cervical screening test. Some people don’t have any symptoms but still get a positive test.
If you have a positive cervical screening test, your doctor may refer you for more tests. You may also need tests if you have symptoms of cervical cancer. Tests may include:
- colposcopy — a specialist doctor looks at your cervix with a magnifying tool to look for abnormal cells that could be cancerous
- biopsy — a sample of your cervix is taken and checked under a microscope for cancer cells
- blood tests — to check how well your kidneys and liver are working and check your general health
- imaging scans — a CT scan or MRI scan can look for signs of cancer or see if it has spread
ASK YOUR DOCTOR — Preparing for an appointment? Use the Question Builder for general tips on what to ask your GP or specialist.
How is cervical cancer treated?
The treatment depends on whether the changes in the cervix are precancerous or if cancer has already formed. ‘Precancerous’ means that the cells in the cervix have started to change but haven't turned into cancer yet.
Treating precancerous cell changes
If tests show precancerous cell changes, your doctor can treat them to stop them from becoming cervical cancer. There are several ways to treat precancerous cells, such as:
- wire loop excision (LLETZ or LEEP) — a thin wire loop heated with electricity is used to remove the abnormal cells from the cervix
- cone biopsy — the area of abnormal cells is removed using a scalpel
- laser surgery — a hot light (laser) shone through the vagina is used to destroy abnormal cervical cells
Treating cervical cancer
If precancerous cells are not treated, they can develop into cervical cancer. If found early, they are often successfully treated with surgery.
Procedures and surgeries to treat cervical cancer include:
- cone biopsy — removes a cone-shaped piece of tissue around early-stage cancer with a scalpel.
- trachelectomy — involves removing the upper part of the vagina and part or all the cervix. This may be an option if you want to have children after treatment.
- hysterectomy — involves removing the uterus, cervix and the top of the vagina. It is the most common surgery for cervical cancer. After this surgery, you won’t be able to become pregnant.
If you have a hysterectomy, at the same time you may also choose to have a bilateral salpingectomy (which involves removing both fallopian tubes) or a bilateral salpingo-oophorectomy (which involves removing both fallopian tubes and both ovaries). If your ovaries are removed before menopause, you will go into sudden menopause.
If cervical cancer has spread to other parts of the body (metastasis), you may need other cancer treatments. These treatments may include radiotherapy or chemotherapy.
Your doctor will consider several factors when recommending the best treatment for you, including:
- the size of the cancer and how far it has spread (its stage)
- your age and overall health
- whether you have gone through menopause
- whether you would like to be able to get pregnant in future
Living with cervical cancer
Treatment for cervical cancer can lead to changes in your bladder, bowel and sexual function. Vaginal dryness is also common after many of the procedures used to treat cervical cancer.
Often, these problems will get better on their own over time. Some people may need extra treatment or support from their healthcare team.
If you are struggling, make sure to ask your doctor for advice and support.
What are the complications of cervical cancer?
Cervical cancer can cause different complications, especially if it spreads to other parts of the body. Treatments may also lead to complications. Here are some of the possible complications.
Metastasis
As with many other cancers, cervical cancer can spread to other parts of the body. This can cause serious complications. If cervical cancer is caught and treated early, the expected outcome is usually good.
Problems with fertility
Treatments for cervical cancer can make it harder to become pregnant or carry a pregnancy to term. Minor surgical procedures on the cervix may increase your chance of miscarriage in future pregnancies.
Surgeries such as removing the uterus, fallopian tubes, or ovaries may mean that you won’t be able to become pregnant.
If being able to become pregnant is important to you, talk to your doctor about your options.
Side effects of cancer treatments
Cancer treatments, including surgery, chemotherapy and radiotherapy, can cause side effects. Your healthcare team will help you manage these.
Can cervical cancer be prevented?
There are ways to reduce your risk of cervical cancer through vaccination and regular screening. These steps can help catch any problems early.
HPV vaccination
The HPV vaccine is available for free to people aged 12 and 13 years through the National Immunisation Program. It helps prevent infections from high-risk types of HPV that can cause cancer.
Cervical screening tests
It is recommended to have a cervical screening test every 5 years if you:
- are aged between 25 and 74
- have a cervix
- have ever had sexual contact
Cervical screening tests have replaced Pap smear tests. They check for high-risk types of HPV by taking a sample of cells from the cervix. This helps find and treat early changes in the cervix that could lead to cancer.
Self-testing for cervical screening is now widely available. This means that you may be able to use a swab to take your own sample. Self-testing isn’t suitable for everyone, so speak to your doctor about what’s right for you.
Resources and support
Find out more about the HPV vaccine in Australia and the National Cervical Screening Program.
For information and support services:
- Cancer Council offers information about cervical cancer and cancer treatment.
- Cancer Australia provides information about cancer and cancer treatment.
- CerviCAN support program supports Australian females with cervical cancer and their families.
- Peter MacCallum Cancer Centre provides cancer information and support services.
- Carers Australia offers information and support for carers.
Aboriginal and/or Torres Strait Islanders
The Cancer Institute NSW has information about cervical screening for Aboriginal and/or Torres Strait Islanders.
The Department of Health, Disability and Ageing offers information about cervical screening in Aboriginal and Torres Strait Islander languages.
Other languages
The Department of Health, Disability and Ageing offers information about cervical screening in multiple languages.
Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: November 2023


















