Basal cell carcinoma (BCC)
Key facts
- Basal cell carcinoma (BCC) is a type of skin cancer and the most common type of cancer.
- BCCs usually develop on parts of the body exposed to the sun.
- They grow slowly so it may take time before you notice one.
- BCCs are usually curable — there are many different treatment options.
- You can help prevent BCCs by protecting your skin from the sun.
What is basal cell carcinoma?
Basal cell carcinoma (BCC) is the most common type of cancer worldwide. It's usually the least dangerous type of skin cancer. BCCs often appear on the skin of the:
- face
- neck
- back
- shoulders
BCCs start in the cells of the top layer of the skin, called the epidermis. They grow slowly over months or years and rarely spread to other parts of the body.
What are the symptoms of basal cell carcinoma?
BCCs often start as a small change in the skin, such as a bump or a flat red patch. They most often happen on parts of your body that get a lot of sun. They may become larger and more noticeable over time.
Signs of BCC include:
- a red or pearly lump or scaly area
- a sore that doesn't heal or gets better and then comes back
- a sore that bleeds
- a mole, scar or dermatitis that bleeds
CHECK YOUR SYMPTOMS — Use the Symptom Checker and find out if you need to seek medical help.
What causes basal cell carcinoma?
BCC is mainly caused by skin damage from ultraviolet (UV) radiation from the sun.
People with fair skin, light hair or who burn easily are more at risk. Other causes include:
- getting older
- repeated sunburns
- use of tanning beds
- some medicines that make your skin more sensitive to UV radiation
- exposure to radiation or arsenic
- a weak immune system
- a family history of skin cancer
What are the types of basal cell carcinoma?
There are several types of BCC, including:
- nodular BCC — the most common type. It usually looks like a pink or pearly bump.
- superficial BCC — usually looks like a flat, pink, scaly patch. It may be mistaken for a rash or eczema.
- morpheaform BCC — a less common but more aggressive type. It usually looks like a firm, ivory-coloured or shiny scar with unclear edges.
There are also several subtypes of BCC.

When should I see my doctor?
See your doctor if you notice a new spot or an existing one that changes size, shape or colour.
Most people notice BCCs by checking their own skin. See a doctor if you find a spot, blemish, freckle or mole that:
- looks different from other spots on your skin
- has changed size, shape, colour or texture
- doesn't heal
- is itchy or bleeds
ASK YOUR DOCTOR — Preparing for an appointment? Use the Question Builder for general tips on what to ask your GP or specialist.
How is basal cell carcinoma diagnosed?
If you notice any changes to your skin, your doctor will examine it. They may take a small sample (biopsy) to test in the laboratory to check if it's a BCC.
Your GP may treat the BCC or may refer you to a dermatologist (skin specialist) for more tests or treatment.
How is basal cell carcinoma treated?
BCCs can almost always be successfully treated. Treatment will depend on:
- the type of BCC
- the size of BCC
- the location of BCC
- your age
- your health
If the BCC was removed during a biopsy, you may not need more treatment.
Surgery
Surgery is the most common treatment. It involves cutting out the BCC and nearby skin. The removed skin is checked to make sure no cancer cells remain in the surrounding skin. If cancer cells are found, you may need more surgery.
Mohs micrographic surgery is a special type of surgery. It removes the BCC layer by layer while checking each layer under a microscope. This helps make sure all cancer cells are removed. Ask your doctor if Mohs surgery is right for you.
Other treatment options
Other BCC treatments include:
- freezing the area with liquid nitrogen (cryotherapy)
- scraping off the spot and sealing the wound with a low-level electric current
- creams, liquids and lotions that help your immune system destroy the BCC (immunotherapy)
- photodynamic therapy — using a light and special cream to treat the BCC
- chemotherapy ointment or cream for skin cancers on the top layer of skin
- radiotherapy — for certain BCCs that can't be removed with surgery
FIND A HEALTH SERVICE — The Service Finder can help you find doctors, pharmacies, hospitals and other health services.
Living with basal cell carcinoma
After treatment, it's important to keep an eye on your skin. If you've had one BCC, you are more likely to get another.
See your doctor or dermatologist for skin checks every 6 to 12 months. Check your own skin regularly and tell your doctor if you notice any new or changing spots.
What are the complications of basal cell carcinoma?
If not treated or fully removed, BCCs can grow and damage nearby tissue. In rare situations, BCCs can spread to lymph nodes or other parts of the body.
Can basal cell carcinoma be prevented?
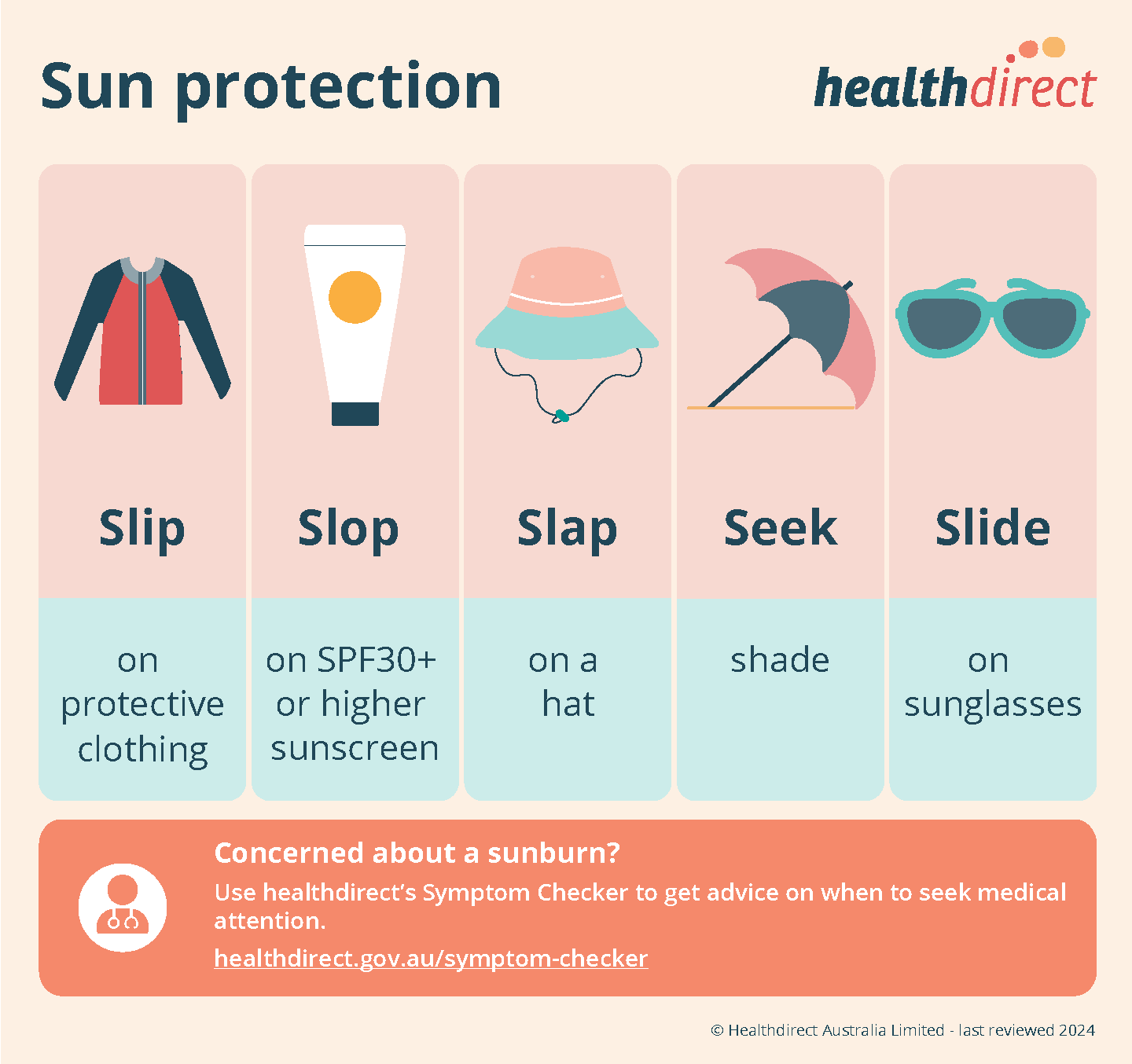
The best way to prevent BCCs is to protect your skin from the sun.
Here are some tips:
- Avoid going out in the sun when the UV Index is above 3 (check the SunSmart app).
- Stay in the shade.
- Wear a hat, sunglasses and clothing that protect you from the sun.
- Use an SPF30+ (or higher) sunscreen.
- Don't use tanning beds.
Resources and support
- Visit Cancer Council for tips on how to check your skin.
- SunSmart has information about how to protect yourself from the harmful effects of sun exposure.
- The Australasian College of Dermatologists has information about Basal Cell Carcinoma.
- The Bureau of Meteorology UV Index has information about the UV index throughout the day and when to stay out of the sun.
- To find a skin clinic near you, use the healthdirect Service Finder
You can also call the healthdirect helpline on 1800 022 222 (known as NURSE-ON-CALL in Victoria). A registered nurse is available to speak with you 24 hours a day, 7 days a week.
Languages other than English
- Cancer Council has information on BCC diagnosis and treatment in several languages.
Information for Aboriginal and/or Torres Strait Islander peoples
- Visit one of the following for information and support on skin cancer for Aboriginal and/or Torres Strait Islander people:
Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: July 2025















