Gastrointestinal bleeding
Call triple zero (000) for an ambulance or go to your nearest emergency department if you:
- vomit blood or material that looks like coffee grounds
- have black, tarry stools (poo) or a lot of blood mixed in with your poo or in the toilet bowl
- have any bleeding and feel lightheaded or weak
Key facts
- Gastrointestinal (GI) bleeding is bleeding from anywhere in your gastrointestinal tract.
- There can be a small amount of bleeding over time, or sudden, serious bleeding.
- GI bleeding may cause you to vomit blood, pass blood in your stools (poo) or have black, tarry stools.
- There are many causes of GI bleeding, including haemorrhoids, a peptic ulcer and diverticular disease.
- GI bleeding can be life-threatening and emergency hospital treatment may be needed.
What is gastrointestinal bleeding
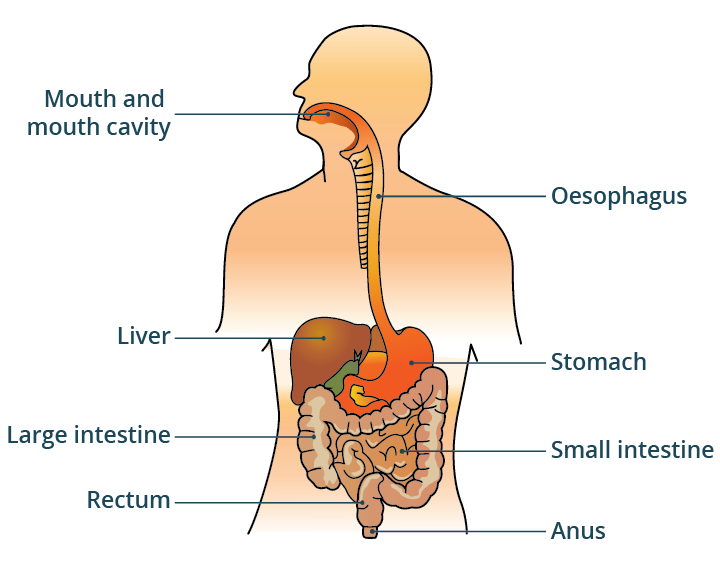
Gastrointestinal (GI) bleeding is bleeding from anywhere in your gastrointestinal tract. That means, anywhere from your mouth to your anus.
There can be:
- a small amount of bleeding over time
- slight bleeding that comes and goes
- sudden, serious bleeding
GI bleeding may cause you to vomit blood or pass blood in your stools (poo).
GI bleeding is a serious symptom and can be life-threatening. Serious or sudden GI bleeding is also called a gastrointestinal haemorrhage.
What symptoms are related to gastrointestinal bleeding?
The symptoms of GI bleeding will depend on:
- where the bleeding is coming from
- how quickly you are bleeding
- how much blood there is
You may be bleeding from your:
- oesophagus (food pipe)
- stomach
- small bowel (intestine)
- large bowel (intestine)
- rectum
- anus
Upper GI bleeding
If you are bleeding from the top part of your GI tract — your oesophagus, stomach or the first part of your small bowel (the duodenum), you may:
- vomit blood that is bright red (called haematemesis)
- vomit blood that looks like coffee grounds
- feel sick (nausea)
- have abdominal pain
- pass black, tarry stools (called melaena)
Rarely can upper GI bleeding cause bright red blood to pass from your back passage (rectum). This is called haematochezia.
Lower GI bleeding
Bleeding from the lower part of your GI tract — your bowel, rectum (back passage) or anus — can lead to passing blood from your back passage. You may have:
- blood mixed in with your stool (poo)
- dark-red coloured stools
- blood in the toilet
- blood on the toilet paper after you wipe
Other symptoms that can be associated with lower GI bleeding are:
- diarrhoea
- constipation
- abdominal pain
- anal pain
- a change in bowel habit
- recent weight loss
Symptoms of blood loss
If you lose a lot of blood quickly, you may:
- feel lightheaded or faint
- feel weak
- look pale and sweaty
- have cold, clammy skin
- have a fast heart rate and low blood pressure
- feel agitated or confused
If you have symptoms of rapid blood loss, call tripe zero (000) straight away for an ambulance.
If you have been bleeding a small amount for a few weeks or months, you may have anaemia. This can make you feel tired, breathless and weak.
CHECK YOUR SYMPTOMS — Use the Symptom Checker and find out if you need to seek medical help.
What causes gastrointestinal bleeding?
There are many causes of GI bleeding.
Upper GI bleeding
Bleeding from your oesophagus, stomach or duodenum can be caused by:
- a peptic ulcer in your stomach or duodenum — these are usually caused by infection with a bacterium called helicobacter pylori
- inflammation and erosions in your oesophagus, stomach or duodenum — this can be related to gastroesophageal reflux disease (GORD)
- varices — enlarged blood vessels — in your oesophagus or stomach
- a tear in the wall of your oesophagus
- cancer in your oesophagus or stomach
Young children may have upper GI bleeding after accidentally swallowing button batteries.
Lower GI bleeding
Bleeding from your bowel, rectum or anus can be caused by:
- diverticular disease — the most common cause of lower GI bleeding in older people
- haemorrhoids
- angiodysplasia — a blood vessel abnormality in your bowel
- bowel ischaemia — when the blood supply to your bowel is blocked
- inflammatory bowel disease — Crohn's disease or ulcerative colitis
- some bowel infections
- bowel cancer or polyps
- anal fissure
Another cause of lower GI bleeding is after having a bowel polyp removed during a colonoscopy.
Risk factors
You may be at increased risk of GI bleeding if you:
- have liver cirrhosis — which can cause varices (dilated blood vessels) in your oesophagus
- drink a lot of alcohol
- are taking anti-inflammatory medicines (NSAIDS), especially if you also take corticosteroid medicines
- are taking blood-thinning medicines — these can increase your risk of bleeding and lead to serious bleeding
- have a blood clotting disorder
How is the cause of gastrointestinal bleeding diagnosed?
Your doctor will want to diagnose the cause of your bleeding and find out how serious it is. You may need urgent hospital treatment.
Your doctor will ask about your symptoms and examine you. They will want to know:
- when you first noticed the bleeding
- how often you have seen blood
- whether you have any other symptoms
- about your general health
- if you have had a recent procedure or endoscopy
- what medicines you are taking
Your doctor will check your pulse, blood pressure and temperature. They will do a general examination, including feeling your abdomen (tummy).
They will also ask you if they can examine your back passage to look for blood. This involves the doctor inserting a gloved finger into your back passage.
Your doctor may organise tests, such as:
- blood tests
- stool tests
- a faecal occult blood test — to check for blood in your stools
- an upper GI endoscopy — where a long, thin, flexible tube with a small camera on the end is used to look at your oesophagus and stomach
- a colonoscopy — where an endoscope is used to look inside your back passage and large bowel
- a CT scan of your abdomen
FIND A HEALTH SERVICE — The Service Finder can help you find doctors, pharmacies, hospitals and other health services.
When should I see my doctor?
See your doctor if you have been feeling unusually tired, breathless or weak.
See your doctor as soon as possible if you have noticed any bright red blood when you open your bowels (do a poo). You may notice this on the toilet paper.
ASK YOUR DOCTOR — Preparing for an appointment? Use the Question Builder for general tips on what to ask your GP or specialist.
When to seek urgent care
Call triple zero (000) for an ambulance or go to your nearest emergency department if you:
- vomit blood or coffee ground material
- have black, tarry stools or a lot of blood mixed in with your poo or in the toilet bowl
- have any bleeding and feel lightheaded or weak
How is gastrointestinal bleeding treated?
Treatment to stop the GI bleeding will depend on the cause.
If you have sudden loss of a lot of blood, you will need emergency treatment. This can include:
- intravenous (IV) fluids given through a drip
- a blood transfusion
- medicines to help stop the bleeding
- an emergency endoscopy or colonoscopy to find the source of bleeding and stop the bleeding
In some cases, surgery may be needed.
What are the complications of gastrointestinal bleeding?
GI bleeding can be very serious. It can be life-threatening if you lose a lot of blood quickly.
Anaemia is a complication of slow GI bleeding.
Can gastrointestinal bleeding be prevented?
You should avoid overusing NSAID medicines, which can lead to GI bleeding.
Also, talk to your doctor about treatment for reflux symptoms (such as heartburn) if you have them.
It's possible to reduce your risk of some conditions that can cause GI bleeding with lifestyle measures. These can include:
- eating a healthy diet with plenty of fibre and daily fluids
- limiting your use of alcohol
- avoiding or quitting smoking
- maintaining a healthy weight
The National Bowel Cancer Screening Program (NBCSP) offers free screening to all Australians aged between 45 and 74 years. The screening test can find microscopic amounts of blood in your stool (poo) sample. This can detect bowel cancer at an early stage, when it can be treated more easily.
Resources and support
The Gastroenterological Society of Australia (GESA) has information on gastrointestinal conditions including bowel polyps, diverticular disease and inflammatory bowel disease.
You can also call the healthdirect helpline on 1800 022 222 (known as NURSE-ON-CALL in Victoria). A registered nurse is available to speak with 24 hours a day, 7 days a week.
Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: October 2024









