Deep vein thrombosis (DVT)
See your doctor immediately if you have signs of a deep vein thrombosis (red, swollen leg). Call triple zero (000) and ask for an ambulance if you have chest pain, trouble breathing or symptoms of stroke or heart attack.
Key facts
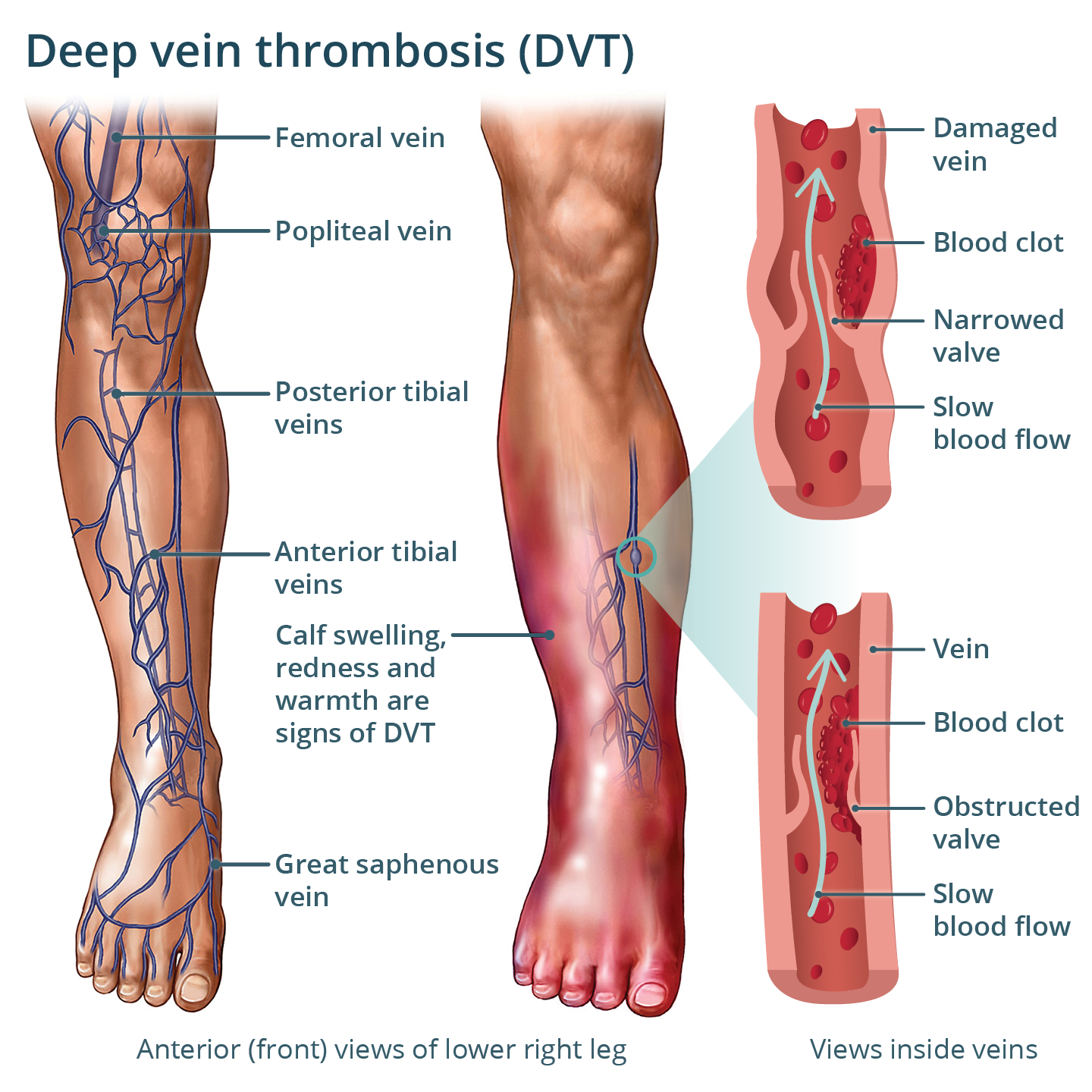
- A deep vein thrombosis (DVT) is a blood clot that occurs in a deep vein, most often in your leg.
- Symptoms of a DVT can include pain and swelling in your calf or thigh.
- A serious complication of a DVT is pulmonary embolism (PE) — when some of the blood clot breaks off and moves through your bloodstream to your lung.
- Blood-thinning medicines are usually used to treat a DVT.
- There are things you can do to reduce your chances of having a DVT.
What is a deep vein thrombosis (DVT)?
A deep vein thrombosis (DVT) is a blood clot that occurs in a deep vein.
DVTs most often affect your legs. But they can occur elsewhere in your body, such as your arms or abdomen (tummy).
What are the symptoms of a DVT?
The main signs and symptoms of a DVT are pain and swelling near the blood clot. This is usually in your calf or thigh. The area may:
- feel sore
- look red or discoloured
- be swollen
- have more noticeable veins (blood vessels) under the skin
Some people have no signs or symptoms. This is called a silent DVT.
CHECK YOUR SYMPTOMS — Use the Symptom Checker and find out if you need to seek medical help.
What causes DVTs?
DVTs are usually caused by:
- slowing of the blood flow in your deep veins
- injuries to your blood vessels
- conditions or other factors that increase blood clotting
Factors that can increase your risk of having DVT are:
- having an injury such as a bone fracture
- being in hospital for surgery or a major illness
- sitting still for a long time, such as during a long-haul flight
- having conditions such as cancer or heart failure
- taking treatments such as the oral contraceptive pill ('the pill') or hormone replacement therapy that contain the hormone oestrogen
- being pregnant
- having a genetic condition that makes your blood more likely to clot
Other factors that can increase your risk include:
- being overweight
- smoking
A DVT can sometimes happen with no obvious cause.
When should I see my doctor?
A DVT is a serious condition. If you think you may have a DVT, you should see your doctor straight away.
Call triple zero (000) for an ambulance if you:
- become short of breath
- have pain in your chest
- have heart palpitations
- feel dizzy or faint
- cough up blood
ASK YOUR DOCTOR — Preparing for an appointment? Use the Question Builder for general tips on what to ask your GP or specialist.
FIND A HEALTH SERVICE — The Service Finder can help you find doctors, pharmacies, hospitals and other health services.
How is a DVT diagnosed?
Your doctor will ask about your symptoms and examine you. They will also ask about your general health and lifestyle.
A blood test called a D-dimer test can be done to help detect blood clots. If you get a positive result, you may need other blood tests.
If your doctor thinks you may have DVT, they may send you for an ultrasound scan or another type of scan.
How is a DVT treated?
The exact treatment for DVT depends on the location of the clot and your risk of complications.
If you have a DVT, you will probably be treated with an anticoagulant (blood thinner) medicine. This will reduce further blood clotting. You might take tablets or have injections. You may need to take blood thinners for several months, or even longer.
You may also need to wear compression stockings.
In rare cases, you may need surgery or a type of medicine called a thrombolytic. This is used to dissolve and break down the blood clot.
What are the complications of a DVT?
Part of the blood clot can break off and travel to your lungs. This is called a pulmonary embolism (PE), which is a serious condition. Symptoms of a pulmonary embolism include chest pain and shortness of breath.
After having a DVT, some people develop 'post-thrombotic syndrome'. This can cause ongoing symptoms in the affected area, such as:
- swelling
- discoloured skin
- pain
- discomfort when you walk
- skin ulcers
Your doctor may recommend wearing compression stockings to help with these symptoms.
Can DVTs be prevented?
There are some steps you can take to help prevent DVTs.
If you are travelling for hours (for example, on planes or trains), remember to:
- get up to walk around every 1 or 2 hours
- do exercises like calf stretches or heel lifts
- drink plenty of water
- avoid alcohol or caffeine as these can add to dehydration
- wear compression stockings if you have other DVT risk factors
When in hospital or recovering from illness, make sure that you:
- tell hospital staff if you have had a DVT before
- wear compression stockings if your doctor has recommended them
- move your feet and legs when possible, even if you are unable to walk around
- stay hydrated
Other general things you can do to help prevent a DVT are:
- quitting smoking
- getting regular physical activity
- maintaining a healthy weight
Resources and Support
Thrombosis Australia has information on blood clots and DVTs.
You can also call the healthdirect helpline on 1800 022 222 (known as NURSE-ON-CALL in Victoria). A registered nurse is available to speak with 24 hours a day, 7 days a week.
Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: May 2025













